Type 2 diabetes is a chronic condition that affects millions of people worldwide. Managing it often requires a combination of medication, diet, and exercise. However, for those with severe obesity, these methods may not be enough to control blood sugar levels effectively. Bariatric surgery has emerged as a powerful tool in the fight against type 2 diabetes, offering significant improvements in blood sugar control and overall health. But which type of bariatric surgery is best for treating type 2 diabetes? In this article, we’ll explore the most common bariatric procedures and their impacts on diabetes management.
The Link Between Obesity and Type 2 Diabetes
Obesity is a major risk factor for developing type 2 diabetes. Excess body fat, particularly around the abdomen, can lead to insulin resistance, where the body’s cells do not respond effectively to insulin. This resistance causes blood sugar levels to rise, leading to type 2 diabetes. Bariatric surgery can help reduce excess weight and improve insulin sensitivity, making it a valuable option for diabetes management.
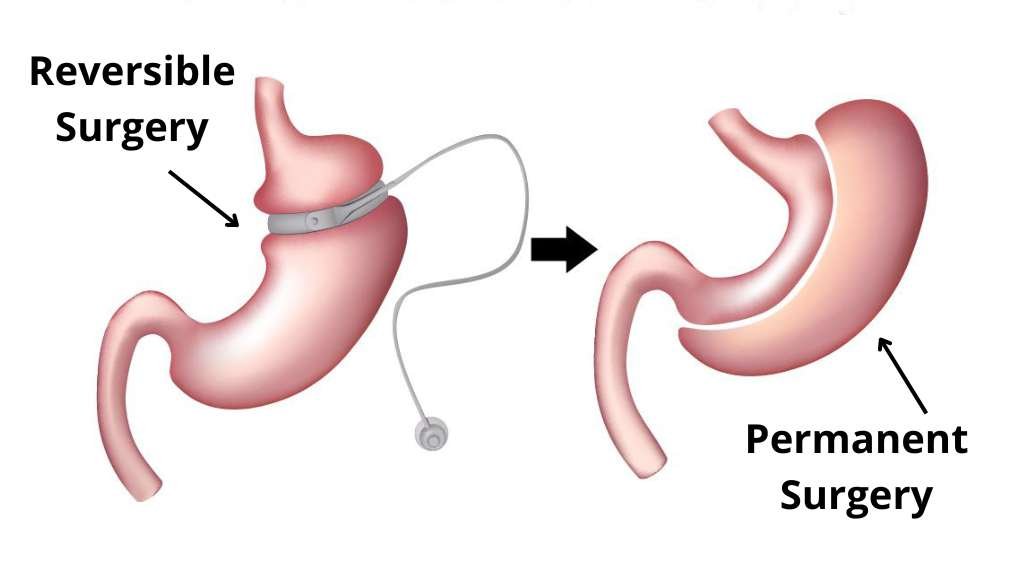
Types of Bariatric Surgery
There are several types of bariatric surgery, each with its unique mechanism and benefits. The most common procedures include gastric bypass, sleeve gastrectomy, and biliopancreatic diversion with duodenal switch (BPD/DS). Let’s take a closer look at each of these surgeries and their effectiveness in treating type 2 diabetes.
1. Gastric Bypass Surgery
Gastric bypass surgery, also known as Roux-en-Y gastric bypass, is one of the most frequently performed bariatric surgeries. During this procedure, the surgeon creates a small pouch at the top of the stomach and connects it directly to the small intestine, bypassing a significant portion of the stomach and the first part of the small intestine.
This surgery reduces the amount of food the stomach can hold and decreases the absorption of calories and nutrients. It also leads to hormonal changes that help improve insulin sensitivity and reduce blood sugar levels.
Studies have shown that gastric bypass surgery is highly effective in improving type 2 diabetes. According to research from Columbia University Medical Center, this procedure has been found to be the best option for weight loss and diabetes control. Patients often experience significant improvements in blood sugar levels, with many achieving remission of diabetes.
2. Sleeve Gastrectomy
Sleeve gastrectomy, or gastric sleeve surgery, involves removing about 80% of the stomach, leaving a tube-like structure. This reduction in stomach size limits the amount of food that can be consumed and helps to decrease hunger by reducing the levels of ghrelin, the hormone responsible for stimulating appetite.
Sleeve gastrectomy has become increasingly popular due to its effectiveness and simplicity compared to gastric bypass. It has also shown promising results in managing type 2 diabetes. A study published by Diabetes UK indicates that sleeve gastrectomy can lead to significant weight loss and improvements in blood sugar control.
3. Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
BPD/DS is a more complex bariatric surgery that involves two steps: first, a sleeve gastrectomy is performed, and then the small intestine is rearranged to bypass a large portion of it. This surgery results in a significant reduction in calorie and nutrient absorption, leading to substantial weight loss.
Although BPD/DS is highly effective for weight loss and diabetes management, it is less commonly performed due to its complexity and higher risk of complications. However, for individuals with severe obesity and poorly controlled diabetes, it can be a viable option. Research highlighted by Everyday Health suggests that BPD/DS can lead to impressive diabetes remission rates.
Benefits of Bariatric Surgery for Type 2 Diabetes
Bariatric surgery offers numerous benefits for individuals with type 2 diabetes, including:
- Improved Blood Sugar Control: Bariatric surgery can lead to significant reductions in blood sugar levels, often allowing patients to reduce or eliminate their need for diabetes medications.
- Weight Loss: All types of bariatric surgery result in substantial weight loss, which helps improve insulin sensitivity and overall metabolic health.
- Reduced Risk of Diabetes-Related Complications: By improving blood sugar control and promoting weight loss, bariatric surgery can reduce the risk of complications such as heart disease, kidney disease, and neuropathy.
- Improved Quality of Life: Patients who undergo bariatric surgery often experience improvements in their quality of life, including increased energy levels and mobility.
Risks and Considerations
While bariatric surgery offers many benefits, it is essential to consider the potential risks and complications. These can include surgical risks such as infection, bleeding, and adverse reactions to anesthesia. Long-term risks may include nutritional deficiencies, bowel obstruction, and the need for additional surgeries.
It is crucial for individuals considering bariatric surgery to undergo a thorough evaluation by a qualified healthcare provider. This evaluation should include an assessment of the patient’s overall health, medical history, and specific needs to determine the most appropriate type of surgery.
Choosing the Right Bariatric Surgery
The decision to undergo bariatric surgery and the choice of procedure should be made in consultation with a healthcare provider. Factors to consider include the patient’s BMI, the severity of their diabetes, their overall health, and personal preferences.
At TurkeyObesity, we specialize in helping patients make informed decisions about bariatric surgery. Our team of experienced surgeons and healthcare professionals provides comprehensive evaluations and personalized treatment plans to ensure the best outcomes for each patient.
Bariatric surgery is a powerful tool in the fight against type 2 diabetes, offering significant improvements in blood sugar control and overall health. Gastric bypass, sleeve gastrectomy, and BPD/DS are all effective options, each with its unique benefits and considerations.
If you are struggling with type 2 diabetes and obesity, bariatric surgery may be the solution you need to achieve better health and a higher quality of life. For more information and to schedule a consultation, visit the TurkeyObesity
FAQs
What is bariatric surgery?
Bariatric surgery refers to a group of surgical procedures designed to help individuals with severe obesity lose weight. These procedures work by reducing the size of the stomach or bypassing parts of the digestive system to restrict food intake and promote weight loss.
How does bariatric surgery help in managing type 2 diabetes?
Bariatric surgery improves type 2 diabetes by enhancing insulin sensitivity and blood sugar control. The surgeries alter gut hormones, which play a crucial role in glucose metabolism, leading to reduced insulin resistance and better glycemic control.
Who is a candidate for bariatric surgery to treat type 2 diabetes?
Candidates typically include individuals with severe obesity (BMI over 35) who have been unable to control their diabetes through lifestyle changes and medication. Candidates should also be committed to making long-term dietary and lifestyle changes post-surgery.
What are the different types of bariatric surgery available for type 2 diabetes?
The main types of bariatric surgery for diabetes include gastric bypass, sleeve gastrectomy, and biliopancreatic diversion with duodenal switch (BPD/DS). Each surgery has unique mechanisms and benefits in terms of weight loss and diabetes management.
Is bariatric surgery safe for treating type 2 diabetes?
Bariatric surgery is generally safe when performed by experienced surgeons in accredited facilities. However, like any surgery, it carries risks and potential complications. Patients should undergo a thorough evaluation to assess their suitability for surgery and understand the associated risks.
What are the benefits of bariatric surgery beyond diabetes management?
In addition to improving type 2 diabetes, bariatric surgery often leads to significant weight loss, which can reduce the risk of other obesity-related conditions such as heart disease, sleep apnea, and joint pain. Patients also report improvements in overall quality of life and mobility.
What lifestyle changes are necessary after bariatric surgery?
Following bariatric surgery, patients must adopt lifelong changes in diet and exercise to maintain weight loss and support their health. This includes consuming nutrient-dense foods, monitoring portion sizes, staying hydrated, and engaging in regular physical activity.
How long does it take to see results from bariatric surgery for diabetes?
Many patients experience rapid improvements in blood sugar levels and may even achieve diabetes remission shortly after surgery. However, individual results vary, and long-term success depends on adherence to post-surgery guidelines and follow-up care.
Are there risks or complications associated with bariatric surgery?
While bariatric surgery is generally safe, potential risks include infection, bleeding, blood clots, and complications related to anesthesia. Long-term risks may include nutritional deficiencies, gallstones, and the need for additional surgeries.
Is bariatric surgery covered by insurance for treating type 2 diabetes?
Insurance coverage for bariatric surgery varies by provider and policy. Many insurance plans cover bariatric surgery for patients who meet specific criteria, such as BMI and documented attempts at non-surgical weight loss.